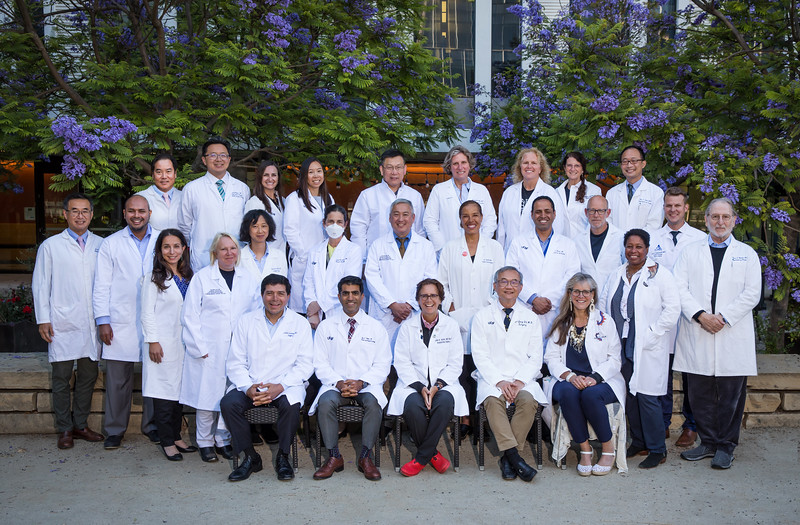
The PCSA 95th Annual Meeting was held on February 9-12, 2024, at the Westin Rancho Mirage Golf Resort & Spa. UCSF help an alumni dinner during the weekend and few Naffziger members were in attendance.
News & Events
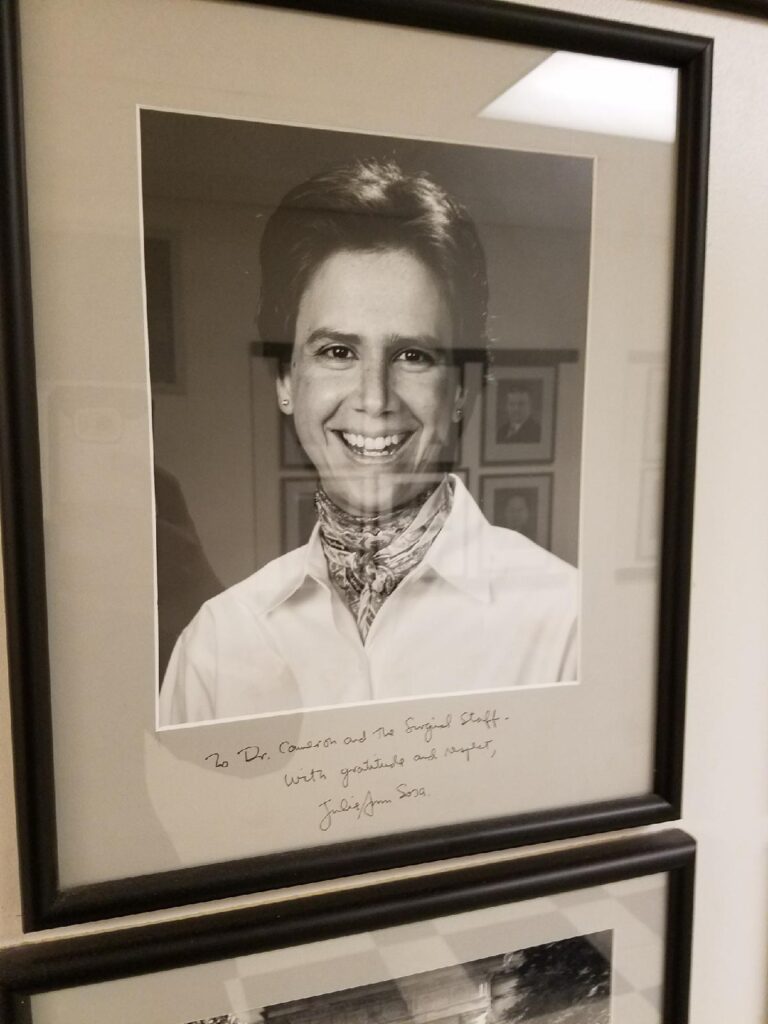
Julie Ann Sosa, MD MA FACS
BIOGRAPHY
Julie Ann Sosa, MD MA FACS is the Leon Goldman MD Distinguished Professor of Surgery and Chair of the Department of Surgery at the University of California San Francisco (UCSF), where she is also a Professor in the Department of Medicine and affiliated faculty for the Philip R. Lee Institute for Health Policy Studies. Dr Sosa came to UCSF in 2018 from Duke. Her clinical interest is in endocrine surgery, with a focus in thyroid cancer. She is an NIH- and FDA-funded investigator and author of more than 400 peer-reviewed publications and 80 book chapters and reviews, all largely focused on outcomes research, health care delivery, hyperparathyroidism, and thyroid cancer, with a focus on clinical trials. She has authored or edited 7 books. Dr Sosa is the immediate Past-President of the American Thyroid Association (ATA) and serves on the Board of Directors/Executive Council of the ATA and International Thyroid Oncology Group; for the ATA, she is chairing the committee responsible for writing the next iteration of differentiated thyroid cancer guidelines. She is the Editor-in-Chief of the World Journal of Surgery and an editor of Greenfield’s Surgery: Scientific Principles and Practice. She has mentored more than 90 students, residents, and fellows, for which she was recognized with induction as a full member to the American College of Surgeons Academy of Master Educators in 2020, and by the ATA with the Lewis E. Braverman Distinguished Lectureship Award in 2017 and its Distinguished Service Award in 2022. She received the Chancellor’s Diversity Award in 2022 for the Advancement of Women at UCSF. Dr Sosa was born in Montreal and raised in upstate New York. She received her AB at Princeton, MA at Oxford, and MD at Johns Hopkins, where she completed the Halsted residency and a fellowship.
1. How did you get interested in endocrine surgery? I spent 6 months during residency on the breast and endocrine surgery service at the John Radcliffe and Churchill Hospitals in Oxford as a specialist registrar and loved it. My Halsted residency training program made me into a pancreatic surgeon but I retooled myself into an endocrine surgeon – and I haven’t looked back!
2. How were you inspired to become a Chair of Surgery and who was your primary mentor to achieve that position? I had the strong sponsorship and encouragement of other women leaders who I’d met through ELAM and (literally) on a bus at a surgical meeting who counseled and supported me along the way. Becoming Chair of Surgery at UCSF is my dream job, and I’m so thankful.
3. You have had a rich and successful research history, what are your current research interests and clinical trials and what area should budding endocrine surgeons be investigating? I love science. My research interests have evolved over time. I continue to do health services research, now focusing more on things like the impact of paid sick leave on health care utilization, and multi-institutional registry work to better understand the natural history of a rare disease (medullary thyroid cancer). Our newest R01 is focused around trying to develop ways to effectively diversify the surgical work force.

Research Resident Profile- Alexis Colley, MD
1. How did you get interested in your research topic?
I first became interested in patient-doctor communication prior to medical school when I was volunteering at a local hospital. There, I began to see the importance of communication in shared decision-making and wondered about how to make things better for surgical patients. Since medical school, my research interests have centered around the role of patient preferences for care and integrating ethics into clinical practice.
In residency, I wanted to understand more about how to align patient preferences and goals with medical and surgical care, which led me to my interest in Advance Care Planning (ACP). ACP discussions can help align treatment intensity with patient preferences to balance the short-term risks vs. longer-term benefits of surgery and post-surgical complication management. I am particularly interested in the components of ACP that can facilitate a shared understanding of patient’s goals and preferences and how surgeons can incorporate that knowledge into their treatment recommendations.
2. How did you select your research mentorship team?
I am lucky to have an incredibly supportive multidisciplinary research mentorship team with Dr. Elizabeth Wick and Dr. Rebecca Sudore. I knew that I wanted to work with Dr. Wick because she is an expert in quality improvement, change management, and organizational culture as it applies to surgery. We were connected via our interest in ACP in surgery to Dr. Sudore, who is a geriatrician, palliative medicine physician, and clinician investigator. Dr. Sudore’s work has focused on improving ACP and medical decision making for culturally and ethnically diverse older adults. With their multidisciplinary expertise, Drs. Wick and Sudore have helped me to look at my research questions from varying perspectives. They have also supported me with my diverse professional interests, particularly advocating for me to take an additional professional development year to complete a clinical fellowship in Palliative Care.
3. How will you incorporate your research into your future career goals?
As a future colorectal surgeon, I see myself practicing in an academic setting where I can continue to work towards integrating palliative care and surgery both in my clinical work and in teaching the next generation of surgeons. Clinically, I plan to have a surgical practice focused primarily on caring for patients with colon and rectal disease, but given my interest in palliative care, I also see myself as caring for patients with a need for a surgical palliative procedure and/or complex decision-making for surgical care. I plan to continue working on improving communication between surgeons, the surgical care team, and patients, including expanding the use of goals and preferences, as well as integrating plain, patient-centered language into surgical consultation.
Research Resident Profile- Nathan Brand, MD
1. How did you get interested in your research topic?
My interest in global health has always been inextricably tied to my interest in global health. As a middle schooler I was introduced to medicine while accompanying my father on medical trips to Nicaragua. In medical school my interest evolved, and I became focused specifically on helping to improve outcomes of cancer patients in low income countries. At UCSF I worked with my mentors Dr. Jablons and Dr. Ozgediz to create a unique research experience spending one year focused on developing novel therapeutics to treat esophageal squamous cell carcinoma, a disease that primarily effects people in low-income countries, and the second year on the ground in Tanzania working on assess the surgical oncology capacity and case volume in Tanzania, a lower-middle-income country in East Africa.
2. How did you select your research mentorship team?
UCSF provided me with an incredible team of mentors with an impressive diversity of expertise. During my rotations as a junior resident, I was introduced to both Dr. Jablons and Dr. Ozgediz. Each mentor was an expert in a specific skillset I wanted to acquire during my research time. The flexible and collaborative culture of UCSF then made it possible for me to pitch to both a non-traditional research experience based partially in the US at a basic science lab and partially in Tanzania working at a medical university.
3. How will you incorporate your research into your future career goals?
In the future, I aspire to become an academic colorectal surgeon with a primary focus on delivering healthcare to underserved patient populations, both within the US and abroad. Through my research experience, I have honed the ability to integrate a scientific and systems-based approach to enhance cancer care. My goal is to contribute by developing innovative treatments and bolstering healthcare systems to ensure that every patient receives the quality medical attention they rightfully deserve.
Naffziger Surgical Society Day & Loupes Day, September 20, 2023

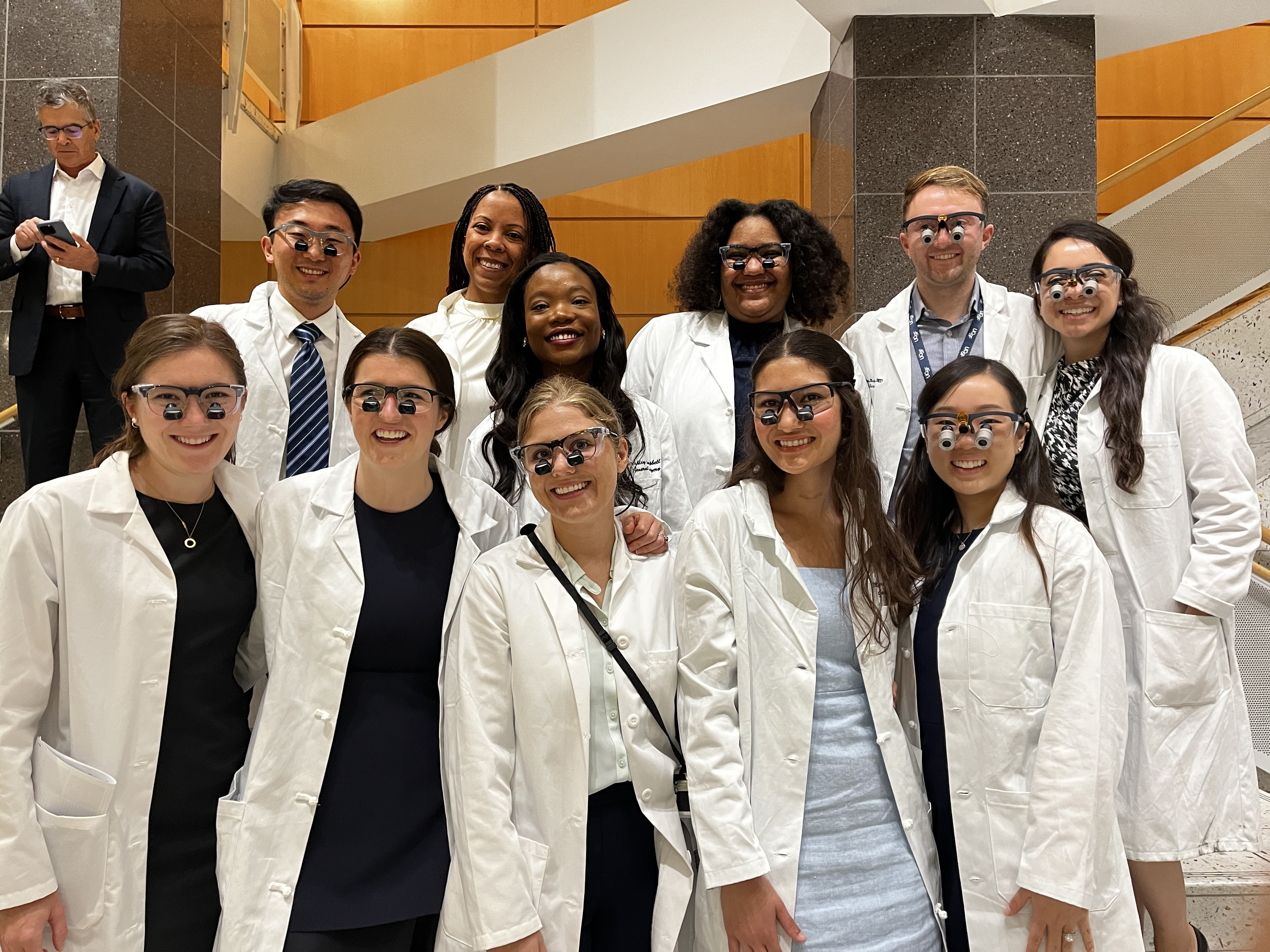

Watch the 2023 NSS Loupes Day Ceremony- Part 1 & Part 2
Research Resident Profile-Audrey Brown, MD MAS
1. How did you get interested in your research topic?
I got really interested in the multidisciplinary nature of treating hepatobiliary malignancies in medical school and wanted to focus my research years on a topic in that space. I was also particularly interested in learning how to manage and analyze large-scale datasets, particularly those involving genomics data. With the help of my primary mentor, Dr. Stock, I put together a project focused on identifying patterns of differential gene expression in cirrhotic liver parenchyma that are associated with Hepatocellular Carcinoma development, which provided the perfect opportunity to marry both of those interests.
2. How did you select your research mentorship team?
I feel so lucky to have had the opportunity to work with truly excellent mentors from multiple different departments at UCSF. My mentorship team included Dr. Peter Stock (Transplant Surgery), Dr. John Roberts (Transplant Surgery)., Dr. Zoltan Laszik (Pathology), Dr. Neil Mehta (Hepatology), and Dr. Emanuela Zacco (Laboratory for Cellular Analysis). While completing a Masters degree in Biostatistics, I was also connected with Dr. Adam Olshen, who specializes in complex transcriptomics analyses and was extremely helpful in guiding my own analysis for this project.
3. How will you incorporate your research into your future career goals?
In my future career, I hope to continue to focus on the applied use of transcriptomic analyses in clinical practice. Several prognostic gene signatures are commonly used in treating patients with breast cancer and colon cancer and I would love to contribute to the devlopment of a similar test for patients with hepatobiliary malignancies.

Naffziger Announces Jennifer Wang, MD, is the Society’s New Vice President
The Naffziger Society is pleased to announce that Jenny Wang, MD is the society’s new Vice President. Dr. Wang completed medical school at Yale School of Medicine & during her residency at UCSF she received a Master’s Degree in Clinical Research, with a focus on outcomes in colorectal surgery. After residency she completed a colorectal surgery fellowship at the Mayo Clinic. Dr. Wang said, “I spent my first 8 years in practice developing the colorectal surgery subspecialty at Kaiser Permanente San Jose and robotic colorectal surgery at Kaiser Permanente Santa Clara”. Read her spotlight questions below:
1. How did you get interested in colorectal surgery?
I had first become interested in IBD following a medical student experience taking care of a very ill teenage girl with UC . I saw her remarkable turnaround after having a total proctocolectomy and J pouch and became interested in surgery and Gi diseases. Colorectal was one of my earliest rotations as an intern at UCSF and I really enjoyed everyone I worked with—they were kind, wonderful people and clearly excited about their work. As I worked more closely with Dr Varma as my research and career mentor, I met other colorectal surgeons at meetings and appreciated the great collegiality within this subspeciality.
2. How you achieved that interest and then evolved it into your current position & Diversity , among other roles?
I worked with Dr. Varma during my research with a focus on pelvic floor diseases and also patient quality of life related to colorectal disease, leading me to pursue fellowship training for colorectal. What I enjoyed most about this subspecialty was the variety of cases (anorectal disease to abdominal operations, open and minimally invasive cases) and also the variety of patients young and old, healthy and sick. I appreciated that most colorectal disease was curable, even earlier stage cancers, and also many surgical treatments could bring signficant improvement in quality of life to patients.
3. Advice to Naffziger members who may want to pursue hospital or medical school leadership positions?
My advice is to continue throughout your career to stay actively involved, not only in patient care but also finding opportunities within your medical system to participate in or lead projects, small or large. Whether you are in academics, community hospital, or group practice, find projects that excite you—whether it is at the local or national level to improve patient care, education, or enhancing relationships among colleagues. It can be easy to fall into a routine of just getting the day to day done, so look beyond the everyday tasks to see the broader picture.
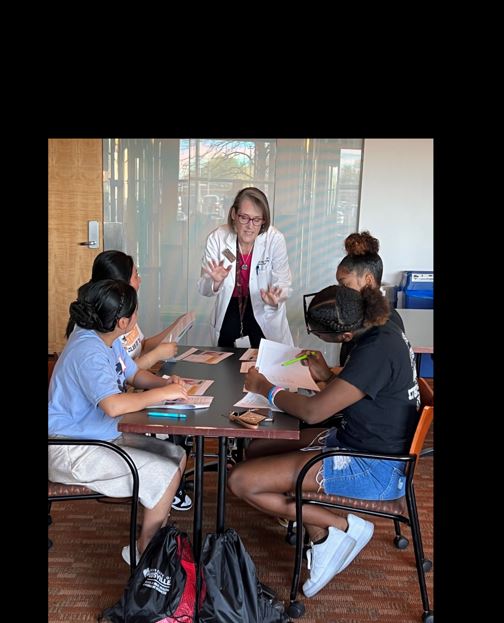
Kelli Bullard Dunn MD FACS
1. How did you get interested in colorectal surgery?
When I was a resident, I loved everything about General Surgery, from Trauma to Transplant. Mentorship was probably the biggest part of my specialty choice of Colon and Rectal Surgery. At CPMC, Drs. Tom Russell, Peter Volpe, Yanek Chiu, and Laurence Yee (who was also a resident ahead of me), and at UCSF Drs. Ted Schrock and Mark Welton really inspired me. Dr. Mika Varma, who was a couple of years ahead of me in residency and then also in fellowship at U of Minnesota was another very positive influence. These individuals showed me that Colorectal Surgery was fun, varied, and (somewhat) controllable in terms of balancing elective vs. urgent/emergent cases. In addition, the specialty allows me to do really big cases and really small cases (and sometimes the small ones can be the most satisfying – like draining a perirectal abscess and seeing a patient feel immediate relief). I also really liked endoscopy, which is a plus. Disease ranges from cancer to benign to functional. CR allowed me to do either basic science research, clinical trials, or outcomes. Finally, it allows me to teach at all levels – medical students (who doesn’t need to learn about hemorrhoids? Yes, we ALL have them!), to residents and fellows, to junior faculty.
2. How you achieved that interest and then evolved into your current position as the Vice Dean of Community Engagement & Diversity, among other roles?
I have been privileged to have worked in all aspects of academic surgery over the course of my career. Early on, I was following the traditional path of a busy clinical practice, leadership in teaching, and running a basic science cancer cell biology lab. I enjoyed all of this tremendously and envisioned myself continuing in this direction for the duration of my professional life. In 2011, I moved to Louisville, KY, and my career changed. In Kentucky, I was immediately struck by the burden of disease and extreme health disparities across the Commonwealth. As such, I approached the Dean of the University of Louisville School of Medicine about creating an office of Community Engagement and Diversity as a way to focus on our stated mission of advancing the health and well-being of our community. I was able to create and grow this office to include both rural and urban health initiatives, workforce “pipeline” programs, and University wide DEI activities. I also began working with community organizations and nonprofits and now hold leadership positions in several. These positions have also given me more opportunities to teach at all levels, from high school students to community leaders, and to raise the profile of the School of Medicine in our region. Finally, I have had the opportunity to serve on a number of University committees and to work with leaders from other schools and colleges, giving me experience in university administration and the “inner workings” of higher education. As a surgeon, I like to work with smart people who are all focused on making things better, whether it is a patient in the trauma room or the learning environment for students. My administrative roles allow me to have influence, and hopefully positive impact, on a wide range of people across my community.
3. Advice to Naffziger members who may want to pursue hospital or medical school leadership positions?
First and foremost, get involved. It is critical that surgeons have a voice in administrative decisions and institutional mission. One of the characteristics of surgeons is the ability to build and lead teams, and to make hard decisions with incomplete information. These qualities are invaluable in hospital and medical school leadership. Early on, I served as a course director and then on a number of hospital committees, including the Scientific Review Committee, Faculty Development Committee, and in Cancer Center leadership. Later I took on more formal administrative roles, first as a Senior Associate Dean and now as a Vice Dean. That said, it is difficult to maintain a busy clinical practice, especially one that is productivity driven, and fulfill myriad administrative responsibilities. It is critical to find a practice that values your administrative time and to have supportive clinical partners. Finally, mentors are crucial throughout your career. Reach out to people in your institution and across the country that are doing what you want to do (or think you might want to do). Figure out what leaves you feeling fulfilled and do that. Take your innate surgical leadership skills to where they are really needed!

Naffziger New Member Picnic
We welcomed the graduating 2022-2023 Chiefs into the Naffziger Society on Saturday, June 10, 2023, 12-3p in Golden Gate Park. The location this year was the Strawberry Hill Top.
Research Resident Spotlight-Simon Chu
How did you get interested in your research topic?
My interest in the field of genome editing dovetails with my passion for surgery as both disciplines allow me to think critically about problems and how to fix them, be it modifying the DNA code or mending tissues. I was amazed by the ability of genome editing and engineering to precisely alter specific genes, be it to cure disease-causing mutations or to impart new functions to cells. My current research focus applies these techniques in finding a cure for Alpha-thalassemia major, a rare blood disorder resulting from deletion of the alpha-globin gene, and in improving the safety and efficacy of stem-cell derived islet transplants.
How did you select your research mentorship team?
During my research time, I was really interested in linking up with surgeon-scientists and PhD scientists in the department that I felt were doing exciting and novel work. I am fortunate to have a mentorship team with Dr. Tippi MacKenzie and Dr. Kyle Cromer, who are both experts in the field of gene editing and offer me invaluable guidance and support. I have benefited greatly by having mentorship by both surgeons and PhD scientists, who have taught me the unique and varied skillset needed to be be a successful surgeon-scientist.
How will you incorporate your research into your future career goals?
My dream is to combine the fields of genome engineering and transplantation towards an independent career as a solid organ transplant surgeon-scientist. I see incredible opportunities in applying genome engineering technology in transplant surgery – from developing stem-cell derived beta cell therapies that could one day replace the need for pancreas transplants, to genetically engineering immune cells to impart precision immunosuppression and supplant the need for morbid immunosupressive agents, the sky’s really the limit!