
Note: The following is a reproduction for the web of a journal article, “The Department of Surgery, University of California, San Francisco by Pamela Derish M.A. and Nancy L. Ascher, M.D., Ph.D. The article spans the history of the Department from the 1860s to 2005. The article is reprinted from Arch Surg/ Vol 140, Dec 2005 www.Archsurg.com with permission from the American Medical Association, 2005;40: 1143-48.
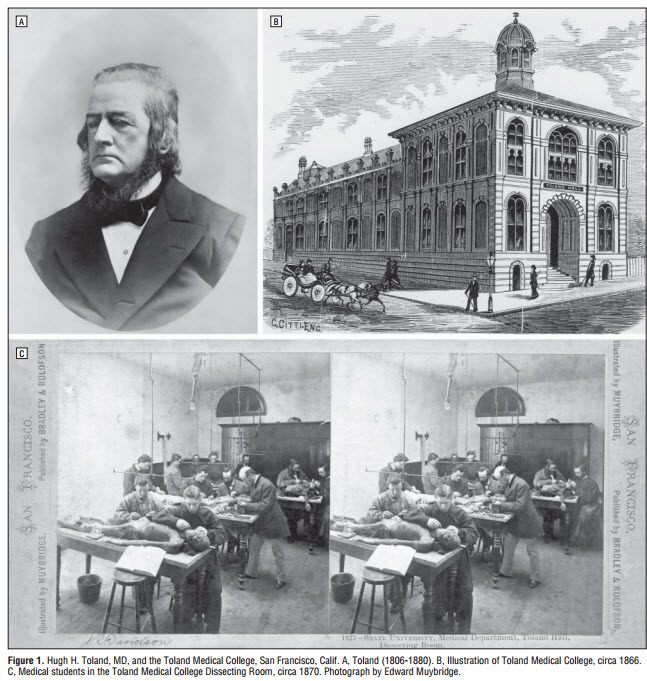
The Department of Surgery at the University of California (UC), San Francisco, was shaped by Gold Rush–era adventurers who stayed on after the gold ran out. In 1852, South Carolina surgeon Hugh H. Toland, MD, was lured to California by gold fever, crossing the 2000-mile overland route by wagon train. By then, gold reserves were declining and the number of miners was increasing dramatically. Whereas many other forty-niners headed home or turned to poker or crime, Toland established an enormously successful surgical practice in the boomtown of San Francisco. He founded the second medical school, Toland Medical College, in the Far West in 1864, timing that coincided with a new state law permitting the use of paupers’ bodies for study by accredited physicians (Figure 1).1
Through the efforts of Richard Beverly Cole, MD—another Gold Rush pioneer and an accomplished surgeon who had arrived in San Francisco aboard a steamship in 1852—the college became the Medical Department of UC in 1873, with Cole as its dean and Toland, the first chair of the Department of Surgery. The early surgical curriculum consisted of “lectures on the principles and practices of surgery, demonstrations of surgical technique on the cadaver, and clinical lectures at the college building and the adjacent county hospital.”2 Anesthesia was scarce, when it was available at all, and Toland, Cole, and the other surgeons performed operations on a table in the middle of the ward. “Blood and noise were the principal features observed by the goggle eyed spectators.”3(p39)
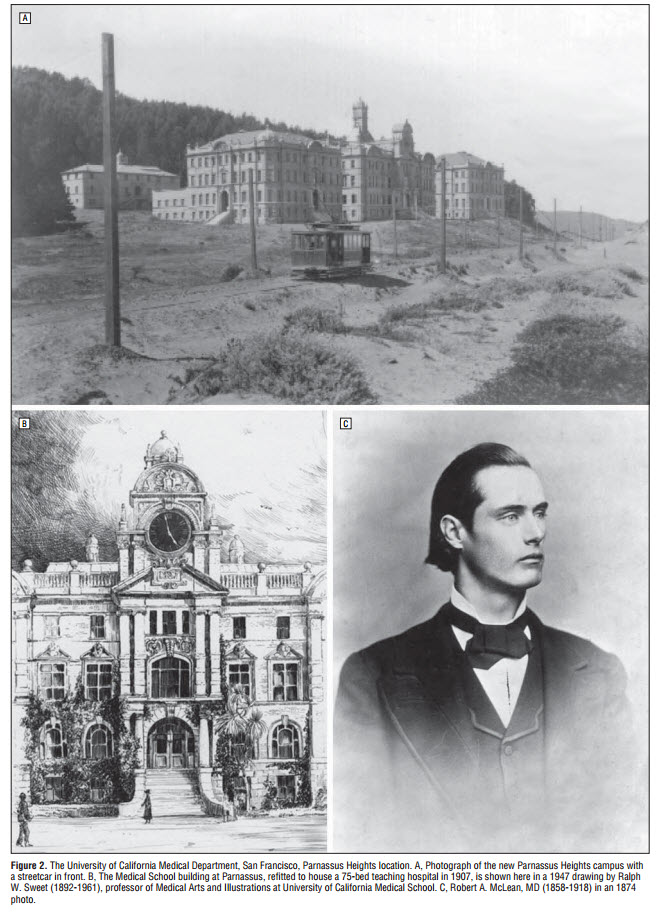
In 1898, the school moved to its present location in Parnassus Heights, overlooking Golden Gate Park. The land was donated by former city mayor Adolph Sutro, in part as an expression of gratitude for the medical education his daughter had received from the “Medical Department” of UC (Figure 2A).2 After the disastrous 1906 earthquake damaged or destroyed most of the city’s existing hospitals, the urgent need for medical facilities necessitated remodeling the medical school building so that it could serve as a hospital. The first UC Hospital opened in 1907 (Figure 2B), under the direction of surgeon Harry Mitchell Sherman, MD.
Toland continued as professor of surgery until his death in 1880. He was succeeded by Robert A. McLean, MD (Figure 2C), a California native, a graduate of Toland Medical College, and professor of anatomy, who introduced formal coursework in the new science of bacteriology into the curriculum. McLean was succeeded in 1899 by Thomas W. Huntington, MD, who had trained at Harvard University (Boston, Mass) and at Massachusetts General Hospital (Boston) before heading west to develop a private surgical practice, treating work injuries, hernias, and appendicitis for railroad companies. In the same year, Huntington performed the first total gastrectomy for carcinoma, after which the patient reportedly survived for many years without evidence of recurrence.2
Wallace I. Terry, MD, another California native, became chair in 1912 when the Medical Department was renamed the UC College of Medicine. By 1915, the college was officially designated the UC Medical School. In a tragic reflection of that time, the last Yahi Indian was found starving in Oroville, Calif. He eventually was brought to live at the UCMuseum of Anthropology at Parnassus, where he was named “Ishi,” the Yahi word for “man.” University of California surgeon and outdoorsman Saxton Pope, MD, (Figure 3A) became his physician and close friend, shooting bows and arrows with him in Golden Gate Park and learning the skills of game hunting.
Pope, who became an expert in Yahi culture, later wrote a book about Ishi’s medical history and several books about archery. During that time, Harold C. Naffziger, MD (Figure 3B), under whose dynamic leadership the department would gain national prominence, had returned to UC to teach and develop a first-class surgical center. Naffziger was born in the mining town of Nevada City, Calif—another legacy of the Gold Rush. He had served as intern and resident surgeon at the UC Hospital and obtained the position of assistant resident surgeon at the Johns Hopkins Hospital in Baltimore, Md, working under William Stewart Halsted, MD, and Harvey Cushing, MD.
While there, Naffziger recognized the superiority of Halsted’s system of training surgeons and became aware of the need for experimental research programs in medical schools.4 Although Naffziger had wide experience in every field of surgery, after World War I, he limited himself to neurological surgery and, with Cushing, was among the very first physicians in America to specialize in this field.4 Naffziger gained national renown for his many distinctive contributions to the new specialty of neurosurgery, including craniotomy decompression for brain tumor, orbital decompression for pressure exophthalmos, and the first partial hypophysection for Cushing disease.5
Naffziger contributed perhaps more than anyone to the national reputation that the UC Medical School now enjoyed. When Naffziger succeeded Terry as chair of the Surgery Department in 1929, he developed a residency program modeled after Halsted’s with the help of H. Glenn Bell, MD, a general surgeon who had been chief resident under another Halsted resident,Mont Reid, MD, in Cincinnati, Ohio. Naffziger wanted residents to experience basic science as part of the curriculum and established the first research laboratory on the Parnassus campus.
In 1947, Naffziger left the Surgery Department to chair UC Medical School’s new Department of Neurological Surgery and Bell became the Surgery Department’s new chair. A superb technical surgeon, Bell emphasized the Halstedian tradition of careful dissection, upgrading the standards of general surgery in California (Figure 3C). He was profoundly interested in the pathologic features of the resected surgical specimens, a habit that he ingrained in his residents, many of whom had a rotation in surgical pathology to enhance their skills in this very important aspect of surgical training. 6
One of those residents was Edwin “Jack” Wylie, MD, a pioneering giant in vascular surgery, who, in 1951, was the first in the United States to perform thromboendarterectomy for atherosclerotic aortoiliac occlusive disease. In 1951, UC established a medical school in Los Angeles, the first of 5 new medical schools in the UC system. The oldest UC Medical School became distinguished as the UC, San Francisco (UCSF).
During the tenure of Leon Goldman, MD, as chair of the Surgery Department from 1956 to 1963, pioneering contributions to vascular surgery continued to be made, including the first axillofemoral artery bypass in 1962. Experimental and clinical gastrointestinal research continued, and some of the earliest transplantation experiments in discordant and concordant species were conducted, which helped set the stage for further investigative and clinical efforts in xenotransplantation. Endocrine surgery was a personal legacy of Goldman.

J. Englebert Dunphy Era
However, additional changes were in store when J. Englebert Dunphy, MD, was recruited from outside the pool of faculty candidates at UC to become chair in 1964. Dunphy, who had trained with Eliot Cutler, MD, one of Halsted’s residents, was a gifted surgeon, an enthusiastic and dedicated teacher, and a scientist with a lifelong interest in the mechanisms of wound healing. He thought development of nascent surgical specialties was being held back by a tradition of conservatism7 and brought in faculty from outside UC. Under his stewardship, pioneering clinical and research activities grew rapidly. 8
Vascular surgery became an independent division. Pediatric surgery began to be defined as a separate specialty, and research was conducted on diaphragmatic hernia, Wilm tumor, and neuroblastoma. The first kidney transplant was performed at UCSF in 1964, and a perfusion machine was developed that successfully preserved donor kidneys for 48 hours, an innovation that made UCSF’s transplantation series one of the most successful in the world. 8
The first cardiac transplant at UCSF was performed in 1969. The Dunphy era also saw the beginning of a research program in wound healing, which continues to receive funding from the National Institutes of Health (NIH), Bethesda, Md, to this day, and the development of the nation’s first organized trauma service at the county hospital, San Francisco General Hospital (SFGH). Innovations were taking place in lower-gastrointestinal surgery, and colonoscopy was brought to UCSF in 1972. Dunphy also integrated residency training into one program involving the San Francisco Veterans Administration ( VA ) Hospital , SFGH, and the University Moffitt Hospital, each of which was developed as a strong teaching and research unit in its own right, led by young and creative faculty. Yet another legacy from the Dunphy era has been the major impact his trainees have had on surgery throughout the English speaking world. For a time, it seemed that the imprimatur of the W.W.B.S. (Worked With Bert Society, one of those never organized but nevertheless important groups) was required for elevation to chairmanship. 9
When Dunphy retired in 1975, he left behind a well-structured department with strong division leaders. 10 His successor, Paul A. Ebert, MD, helped establish UCSF as an international referral center for children with cardiac defects and fostered the development of pediatric cardiac surgery. Congenital heart disease was studied in fetal lambs, myocardial protection with cold ischemic potassium cardioplegia was examined, and clinical studies were done on the operative closure of the patent ductus arteriosis in premature infants. Exciting work using the fetal lamb model to study the physiologic consequences of a surgically created diaphragmatic effect would play a significant role in the development of open fetal surgery (vesicotomy for an infant with urinary obstruction), first performed in 1981 at UCSF. This success was owing to collaboration among UCSF surgeons, obstetricians, and radiologists, all of whom were relatively young junior faculty “who were still naïve enough to think that we could do something that had not yet been seriously attempted.” 11(p518)
In the area of endocrine research, iodine deficiency, hyperparathyroidism, and thyrotropin binding were all being investigated. Vascular surgery research was focused on arterial autografts and visceral arterial atherosclerosis. The role of glycolytic intermediates and ramifications of total parenteral nutrition were studied in collaboration with the Lawrence Berkeley National Laboratory (Berkeley, Calif) and the UCSF departments of Microbiology and Immunology.
After Ebert departed to assume directorship of the American College of Surgeons (Chicago, Ill) in 1986, Haile Debas, MD, a leading expert on the gastrointestinal system who had contributed to understanding the physiologic, biochemical, and pathophysiologic characteristics of gastrointestinal peptide hormones, was recruited to become the next chairman. Research dollars to the department went from 98th place of 125 in the previous decade to ninth in the nation, reaching second place by the early 1990s. A new Center for the Study of Gastrointestinal Motility and Secretion conducted studies in patients with esophageal motility disorders
Transplantation activities accelerated rapidly: the first liver transplant at UCSF was performed in 1988, followed by thoracic organ transplants in 1989, a pancreas transplant in 1989, and a heart-lung transplant in 1991. Laparoscopic surgery also accelerated rapidly, beginning with the first laparoscopic cholecystectomy, performed in 1990, which was followed just months later by the first UCSF laparoscopic cholecystectomy course and expansion of the laparoscopic repertoire to Taylor vagotomies, appendectomies, and the excision of liver cysts. Vascular surgeons began exploring minimally invasive approaches to treating aorticaneurysms.
Wound healing research received a 5-year, $3 million NIH grant to study collagen synthesis and angiogenesis. The newly organized UCSF Fetal Treatment Center began an NIH-funded study of fetal surgery for diaphragmatic hernia and controlling preterm labor. A merger with Mount Zion Hospital (San Francisco), a voluntary, nonprofit hospital in operation since 1887, began a new era in thoracic and oncology surgery when UCSF/Mount Zion became an NIH–funded comprehensive cancer center in 1993-1994. The SFGH campus of UCSF continued to be a major force in improving the care of trauma patient s .
Important clinical advances included using computed tomographic scans to evaluate blunt abdominal injur y and nonoperative management of particular types of liver injuries. 12 San Francisco General Hospital also played a nationally prominent role in the surgical response to the human immunodeficiency virus epidemic, leading the nation in adopting new infectioncontrol procedures for surgery, including double gloving and using waterproof garments and face shields to prevent mucocutaneous exposure to blood.
When Theodore Schrock, MD, assumed the chairmanship in 1993, after Debas was appointed dean of t h e S c h o o l o f Me d i c i n e , ma j o r changes in reimbursements had tightened their grip on the UCSF academic medical center, prompting a merger between UCSF and Stanford University (Stanford, Calif) in 1997. Although historically the 2 institutions had shared the staffing of SFGH and the VA Hospital for decades, this time the 2 faculties failed to come together and the merger was dissolved a year and a half later.
The 1990s were also a time of great expans ion of the department’s already strong laparoscopic surgery efforts. Collaborations with bioengineers were forged to develop virtual-reality software and robotic devices that wo u l d o v e r c ome t h e technical limitations of the instrumentation in current use.
The Center for the Study of Gastrointestinal Motility and Secretion also expanded, and fetal surgery continued full speed ahead. A few of the many milestones of this group included the ex utero intrapartum treatment procedure for airway obstruction in 1995, which has been performed more than 40 times for infants with various types of airway obstruction, such as congenital cystic adenomatoid malformation, cystic hygroma, and tracheal obstruction; completion of an NIHsponsored clinical trial for open repair of a fetus with congenital diaphragmatic hernia in 1996; fetal endoscopic (fetoscopic) surgery in 1996; successful resuscitation of a fetus during open fetal surgery for sacrococcygeal teratoma in 1996; an NIH trial of a fetoscopic balloon for congenital diaphragmatic hernia in 1998; and percutaneous radiofrequency ablation of a sacrococcygeal teratoma in 1999.
Since Nancy L. Ascher, MD, PhD, became chair in 1999, solid organ transplantation has taken place in patients with human immunodeficiency virus, adult live-donor liver transplantation has joined adult-to-child for transplantation procedures, a new center for patient directed breast care has been developed, and a multicenter clinical trial of adjuvant therapy of colorectal cancer has been conducted.
Other important advances over the last 5 years include the development of a novel endovascular treatment for vascular and abdominal vascular disease, fetal endoscopic laser treatment of a single arteriovenous communication in twin-twin transfusion syndrome, and initiation of a pancreas islet program. An affiliation has been established with the East Bay Surgery Residency Program, centered at Alameda County Medical Center (Oakland, Calif).
Today, the mission of the UCSF Department of Surgery is 3-fold: to develop the next generation of leaders in surgery; to provide outstanding quality clinical care that is both compassionate and cost-effective; and to make significant advances in scientific knowledge and clinical practice through both basic and clinical research. The “crown jewel” of our department is our residency program, consistently ranked among the top 10 programs in the nation.
More than 80% of graduates from the past 30 years have continued in fellowship programs, and almost half become surgical academicians associated with university departments of surgery. Residents rotate through our flagship hospital, Moffitt/Long Hospital, a quaternary care center and major university research hospital; SFGH, San Francisco’s municipal hospital and its only level I trauma center; the San Francisco VA Medical Center, a referral center for other regional VA hospitals; the UCSF/Mount Zion Hospital, a regional cancer center; the San Francisco Kaiser Permanente Hospital, a large health maintenance organization; and the California Pacific Medical Center (San Francisco), a privatepractice clinical setting where our residents train with private community-based surgeons.
This combination of hospitals gives residents broader exposure to clinical surgery than any other program in the country. Basic and clinical research by faculty, fellows, and residents is fundamental to our mission. We provide the opportunity for residents to engage in research activities for 2 to 3 years. Surgical residents can work in the laboratories of leading basic science researchers throughout the university. We also offer strong clinical research opportunities in gastrointestinal surgery, transplantation, trauma and sepsis, vascular disease, cancer, fetal treatment, and wound healing. University of California, San Francisco, was the fourth largest recipient of NIH research dollars in 2004, receiving a total of $438.8 million.
The department includes 85 full-time faculty in its 9 divisions, including 15 basic scientists. These divisions, which oversee resident and student education, clinical activities, and research, are Adult Cardiothoracic Surgery, Pediatric Cardiothoracic Surgery, General Surgery, Fetal Surgery, Pediatric Surgery, Plastic and Reconstructive Surgery, Transplantation, Trauma (at SFGH), and Vascular Surgery. Recognized nationally and internationally, our division chiefs and faculty have served as officers of major surgical societies, members of specialty boards, and members of study sections at the NIH. Many of the clinical services and individual faculty are rated as being among the “top 10 in patient care” in the nation.
After 101 years, the Department of Surgery at UCSF continues to value hard work, productivity, and creativity as we strive to improve surgical techniques, make surgery more effective while less invasive, and improve care for patients. In keeping with William Osler’s ethos, we continue to “let each day’s work absorb [our] entire energies.” 13(p10)
Correspondence: Dr Ascher, University of California, San Francisco, 513 Parnassus Ave, S-322, San Francisco, CA 94143-0104 (aschern @surgery.ucsf.edu).
Acknowledgment:We thank Nancy Rockafellar, PhD, of the University of California, San Francisco, Oral History Program, Department of Anthropology, History, and Social Medicine, and Valerie Wheat, BA, MLS, of the University of California, San Francisco, Archives and Special Collections, for help in researching information for this article.
(REPRINTED) ARCH SURG/ VOL 140, DEC 2005 WWW.ARCHSURG.COMCardiothoracic Surgery
1143, ©2005 American Medical Association. All rights reserved.
Downloaded from www.archsurg.com at UCSF/Library, on December 20, 2005
REFERENCES
1. A history of the UCSF School of Medicine. Available at: https://history.library.ucsf.edu. Accessed June 14, 2005.
2. San Francisco: historical overview. University of California History Digital Archives Web site. Available at: https://sunsite3.berkeley.edu/uchistory /general_history/campuses/ucsf/departments_s .html. Accessed June 14, 2005.
3. Blaisdell FW, Grossman M. Catastrophes, Epidemics and Neglected Diseases. San Francisco General Hospital and the Evolution of Public Care. San Francisco, Calif: The San Francisco General Hospital Foundation; 1999:39.
4. In memoriam: Howard Christian Naffziger. University of California History Digital Archives Web site. Available at: https://sunsite.berkeley.edu /uchistory/archives_exhibits/in_memoriam/index3 .html. Accessed June 14, 2005.
5. Rosegay H. A history of neurological surgery at the University of California , San Francisco. Neurosurgery. 1996;38:794-805.
6. In memoriam: H Glenn Bell. University of California History Digital Archives Web site. Available at: https://sunsite.berkeley.edu/uchistory/archives _exhibits/in_memoriam/index3.html. Accessed June 14, 2005.
7. Interviews With J. Englebert Dunphy, MD, UCSF Oral History Program, Department of Surgery Interview Series 4. UCSF Surgery in the Postwar Years. Building an Exemplary Department of Surgery. San Francisco: The Regents of the University of California; 2000:11.
8. Way LW. A festschrift for John Englebert Dunphy, MD. Am J Surg. 1978;135:273-275. 9. In memoriam: J Englebert Dunphy. University of California History Digital Archives Web site. Available at: https://sunsite.berkeley.edu/uchistory /archives_exhibits/in_memoriam/index3.html. Accessed June 14, 2005.
10. Interviews With Paul A. Ebert, UCSF Oral History Program, Department of Surgery Interview Series 5. UCSF Surgery in the Postwar Years. Uniting Pediatric Cardiology and Congenital Heart Surgery. San Francisco: The Regents of the University of California; 2000:xxii.
11. Harrison MR. The University of California at San Francisco Fetal Treatment Center: a personal perspective. Fetal Diagn Ther. 2 0 0 4 ; 1 9 : 513-524. 12. Schecter WP. San Francisco General Hospital. Arch Surg. 2003;138:823-824. 13. Osler W. After twenty-five years. Montreal Medical Journal. November 1899:10. Pamela Derish, MA Nancy L. Ascher, MD, PhD