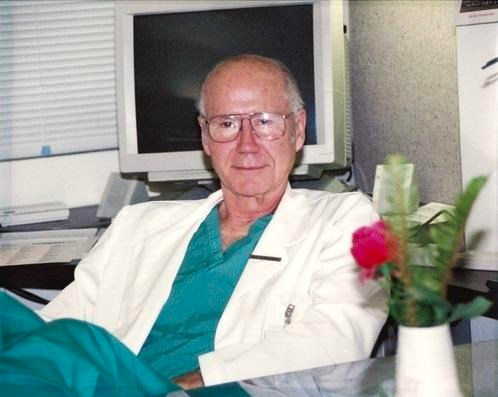
Arthur Norman Thomas, MD
01/27/1931 – 06/29/2025
“Dr. Arthur N. Thomas died at home on Sunday, June 29, at the age of 94. He is survived by his beloved wife of nearly 75 years, Adeline, their five children, seven grandchildren, and three great-grandchildren.
Dr. Thomas chose to become a surgeon at age 13, a decision that shaped a distinguished career spanning six decades. He published more than 125 scientific articles, contributed to several medical textbooks, and was a frequent presenter at surgical conferences.
A pioneer in hyperbaric medicine, Dr. Thomas led early research into the use of hyperbaric environments to enable surgeries requiring extended periods with poor circulation. Soon after, he was awarded a prestigious three-year grant from the National Institute of Health to explore the use of membranous oxygenators for prolonged heart-lung bypass.
Dr. Thomas served as Chief of Thoracic Surgery at San Francisco General Hospital, where he became a member of the first trauma team ever assembled. He spent the rest of his career as Professor of Surgery at the University of California, San Francisco, one of the country’s finest surgical training programs.
His innovative approach to surgery laid the groundwork for today’s surgical procedures for cardiac rhythm disorders and esophageal disorders and injuries. Some 15.8 million Americans each year are affected by these conditions. He co-founded the Samson Thoracic Surgical Society in 1974, later known as the Western Thoracic Surgical Association (WTSA). This professional organization today is a robust institution
with hundreds of members.
Dr. Thomas’s legacy endures in the lives he touched, the students he mentored, and the many contributions he made to the advancement of medicine. A private memorial service will be held by the family.”
Published by San Francisco Chronicle on Jul. 13, 2025.