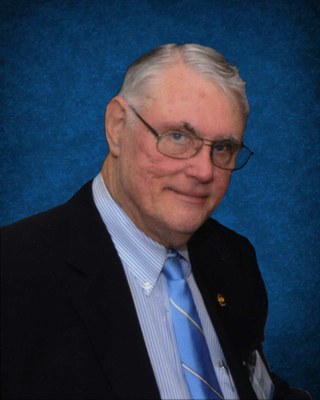
Theodore R. Schrock, M.D., who had a storied career at UCSF, as a medical student, then a surgery resident, faculty member, Department of Surgery Chair and Chief Medical Officer for UCSF Medical Center, recently passed away at age 76.
Theodore (Ted) Schrock was born and raised in Berne, Indiana. He lettered in three sports during high school and was noted for scholarship. He attended Indiana University in Bloomington where he was elected to Phi Beta Kappa and was named “Premed Student of the Year”. His A.B. degree with Highest Honors was obtained after the first year of medical school at UCSF, where, as a senior, Ted was President of the Student Body of the UCSF campus. He was elected to the Alpha Omega Alpha honor society, and upon graduation in 1964, received the Gold Headed Cane as the student who most exemplified the qualities of the true physician. He served as President of the Gold Headed Cane Society for 12 years.
Dr. Schrock entered residency in surgery at UCSF, spent two years as a Research Fellow at Harvard Medical School, and completed residency in 1971. He was immediately recruited to the surgical faculty at UCSF, where he would spend his entire 33-year career in academic medicine. During this time, Dr. Schrock developed an international reputation for excellence in the surgical management of inflammatory bowel disease, serving as a guest lecturer and visiting professor around the globe. His academic milestones included nearly 200 articles, book chapters and abstracts, membership in sixteen professional societies, editorship of two journals: Perspectives in Colon and Rectal Surgery, and of Colon and Rectal Surgery Outlook, and several distinguished service awards.
In 1993, Dr. Schrock was appointed Interim Chair of UCSF Department of Surgery. In three short years, his effective leadership culminated in his permanent appointment as Chair of the Department in 1996. Two years later, he became Chief Medical Officer for UCSF Medical Center, remaining in that position until his retirement in 2004.
Early in his career, Dr. Schrock was a pioneer in the use of colonoscopy as a diagnostic and therapeutic tool for diseases of the colon and rectum, gaining national and international renown for his work. He was a founding member of the Society of American Gastrointestinal Endoscopic Surgeons and became its President in 1988. He was also a key figure in organizing the First World Congress of Surgical Endoscopy in Berlin in 1988, and was an invited participant to numerous world conferences and congresses on these subjects.
Dr. Schrock was also honored as the Gerald Marks Lecturer by the Society of American Gastrointestinal Endoscopic Surgeons. He was the first surgeon to become President of the American Society of Gastrointestinal Endoscopy, and was invited to deliver the Distinguished Lecture to the annual meeting of that society in 1993.
Among his numerous roles at UCSF Medical Center and UCSF School of Medicine, Dr. Schrock was Chair of the Credentials Committee, Vice-President of the Medical Staff, and President of the Medical Staff. He also served as President of the UCSF Howard C. Naffziger Surgical Society for its 1987-88 term.

After retirement, he and his wife bred Arabian horses in Montana, later moving to Scottsdale, Arizona where they lived at the time of Ted’s passing.
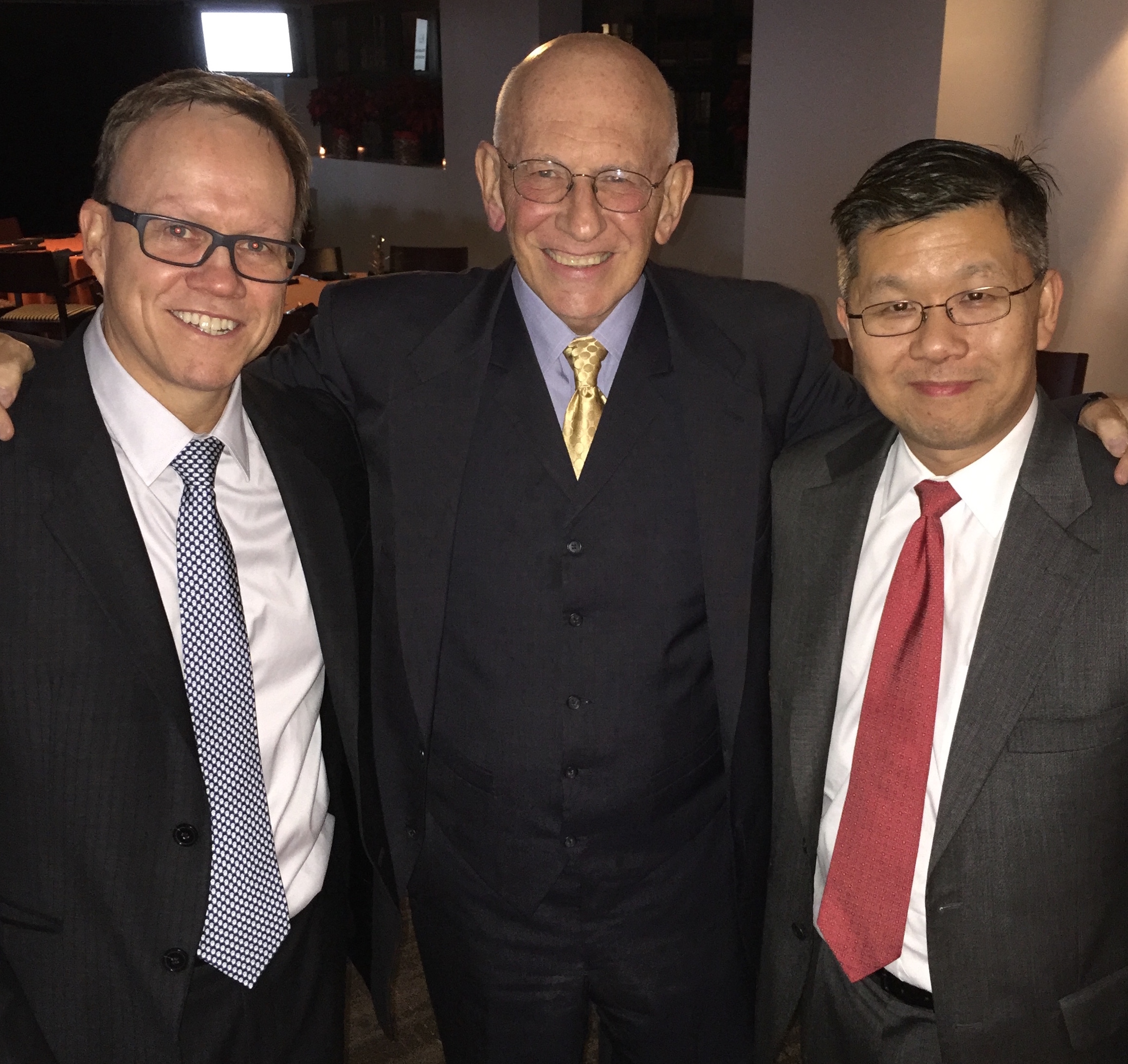
Celebration of Dr. Schrock’s Life
There will be a celebration of Theodore (Ted) Schrock’s life on October 2, 2016, details of which are available at the family posting on CaringBridge.org. Those wishing to attend should visit the family page (registration required).